Published 31 August 2023
Decoding the Culprits: Unveiling Erysipelas Causes for Effective Relief
Understanding Erysipelas
To effectively address the causes and find relief from erysipelas, it is essential to have a clear understanding of this skin condition. This section will explore what erysipelas is and highlight the symptoms and characteristics associated with it.
What is Erysipelas?
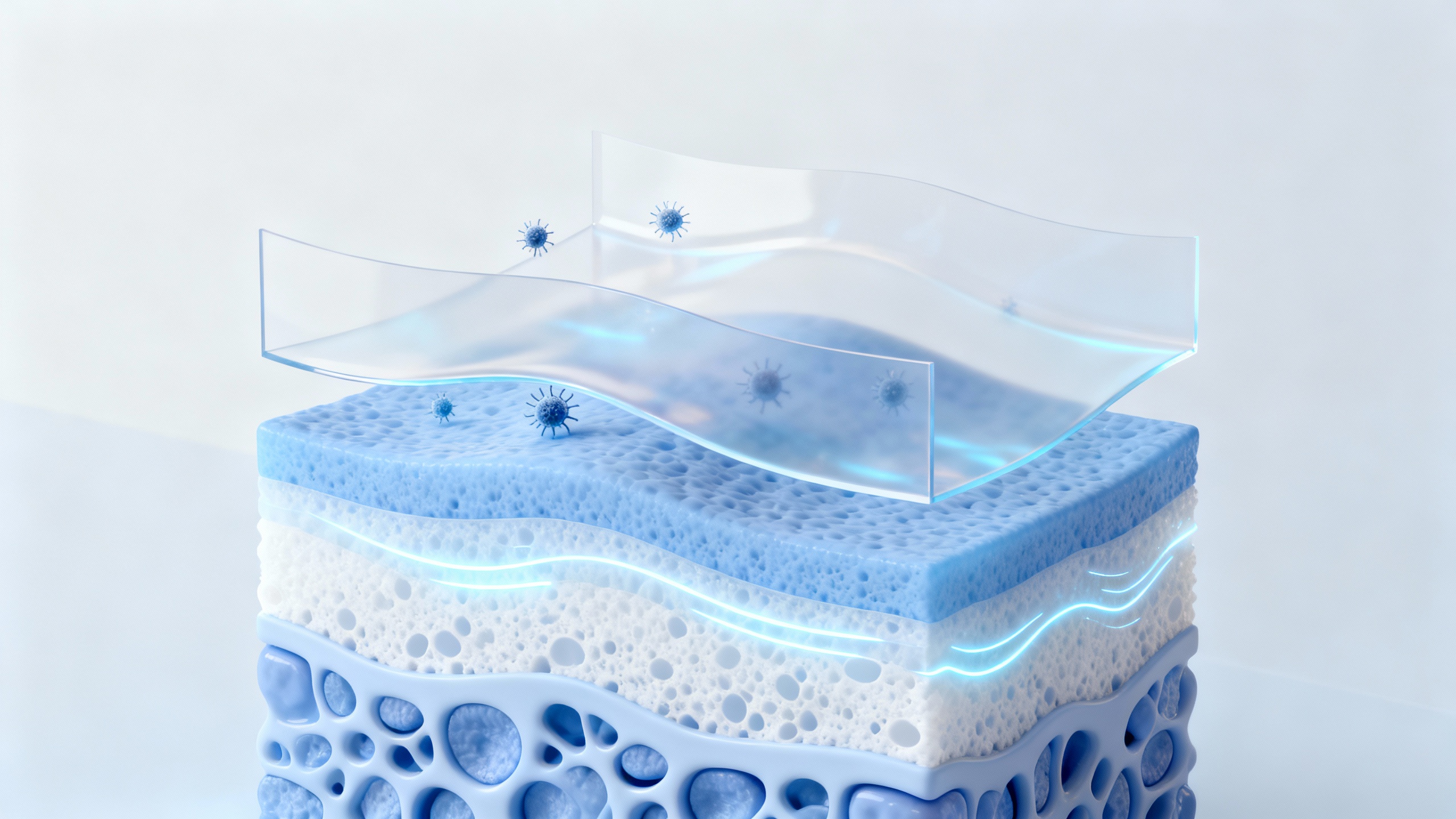
Erysipelas is a type of bacterial skin infection that affects the superficial layers of the skin, primarily the dermis. It is typically caused by the bacteria Streptococcus pyogenes (group A streptococcus) but can also be caused by other types of bacteria. Erysipelas is characterized by red, swollen, and painful lesions that have a sharp border and may feel warm to the touch. These lesions often have a raised appearance and can develop on any part of the body, but they commonly occur on the face, legs, and arms.
Erysipelas is more prevalent in individuals with compromised immune systems, such as those with diabetes, chronic venous insufficiency, or lymphatic disorders. It can also occur in individuals who have experienced skin injuries, such as cuts, burns, or ulcers. Understanding the symptoms and characteristics of erysipelas is crucial in identifying and seeking appropriate treatment for this condition.
Symptoms and Characteristics of Erysipelas
The symptoms of erysipelas can vary, but they generally include:
- Intense redness: The affected area of the skin appears bright red and may have a distinct border.
- Swelling: The skin becomes swollen and may feel tight or stretched.
- Pain and tenderness: The affected area is often painful to the touch and may be tender.
- Warmth: The skin in the affected area feels warm or hot.
- Blisters or rash: In some cases, blisters or a rash may develop within the affected area.
- Fever: Erysipelas can be accompanied by fever, chills, and general malaise.
It’s important to note that erysipelas should be differentiated from other skin conditions with similar symptoms. If you suspect you have erysipelas or are experiencing persistent skin issues, it is advisable to consult a healthcare professional for an accurate diagnosis. Diagnostic tests, such as a physical examination and possibly a bacterial culture, may be conducted to confirm the presence of erysipelas.
By understanding the nature of erysipelas and recognizing its symptoms, individuals can take appropriate measures to address the condition and seek timely medical attention. In the next section, we will delve into the causes of erysipelas, shedding light on the primary factors that contribute to the development of this bacterial skin infection.
Identifying the Causes of Erysipelas
To effectively address and find relief from erysipelas, it is important to understand the underlying causes. The primary cause of erysipelas is a bacterial infection, specifically an infection caused by the bacteria Streptococcus pyogenes. This bacterium enters the body through breaks or cuts in the skin, leading to the development of erysipelas.
Bacterial Infection as the Primary Cause
Erysipelas is primarily caused by a bacterial infection, with Streptococcus pyogenes being the main culprit. This bacterium is commonly found on the skin and mucous membranes. When it enters the body through a break or break in the skin, it can cause an infection, leading to erysipelas. The bacteria can enter the body through even the smallest of cuts, insect bites, or skin injuries.
Common Risk Factors for Erysipelas
While Streptococcus pyogenes is the primary cause of erysipelas, several risk factors increase the likelihood of developing the condition. These risk factors include:
-
Skin injuries and breaks: Any break in the skin, such as cuts, wounds, surgical incisions, ulcers, or even cracks in the skin due to dryness, can serve as an entry point for bacteria, increasing the risk of erysipelas. It is important to promptly clean and treat any skin injuries to reduce the risk of infection.
-
Underlying medical conditions: Certain medical conditions can weaken the immune system or impair skin integrity, making individuals more susceptible to erysipelas. Examples of these conditions include diabetes, lymphedema, venous insufficiency, and chronic skin conditions like eczema or psoriasis. Proper management of these conditions can help reduce the risk of developing erysipelas.
-
Weakened immune system: A weakened immune system due to factors such as underlying medical conditions, immunosuppressive medications, or recent surgeries can increase the risk of erysipelas. It is important to take necessary precautions and follow medical advice to maintain a healthy immune system.
By understanding the causes and risk factors associated with erysipelas, individuals can take preventive measures to reduce the likelihood of developing the condition. Good skin hygiene, prompt treatment of skin injuries, and strengthening the immune system are essential in minimizing the risk of erysipelas. If you suspect you may have erysipelas or are experiencing symptoms, it is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment. For more information on seeking medical attention for erysipelas, refer to our article on when to consult a healthcare professional.
Recognizing Erysipelas Triggers
To effectively manage and prevent erysipelas, it’s crucial to identify the triggers that can contribute to its occurrence. By understanding these triggers, individuals with erysipelas can take proactive measures to minimize the risk of recurrence. Some common triggers include skin injuries and breaks, underlying medical conditions, and a weakened immune system.
Skin Injuries and Breaks
Skin injuries and breaks provide an entry point for bacteria, which can lead to the development of erysipelas. Even minor cuts, abrasions, insect bites, or surgical wounds can create an opportunity for bacteria to penetrate the skin barrier. It’s important to keep all skin injuries clean and promptly apply appropriate treatments to prevent infection. Proper wound care and maintaining good skin hygiene are essential in minimizing the risk of erysipelas. For more information on identifying and treating various skin injuries, refer to our article on identifying skin injuries and treatment.
Underlying Medical Conditions
Certain underlying medical conditions can predispose individuals to erysipelas. Chronic conditions such as lymphedema, diabetes, eczema, and venous insufficiency can compromise the integrity of the skin and impair the body’s ability to fight off infections. It’s important for individuals with these conditions to be extra vigilant in managing their skin health and seeking appropriate medical care when necessary. For more information on identifying and managing underlying medical conditions that can contribute to erysipelas, refer to our articles on lymphedema, diabetes, eczema, and venous insufficiency.
Weakened Immune System
A weakened immune system can make individuals more susceptible to infections, including erysipelas. Factors that can contribute to a weakened immune system include chronic illnesses, immunosuppressive medications, stress, and poor nutrition. Strengthening the immune system through a healthy lifestyle, proper nutrition, adequate sleep, and stress management can help reduce the risk of erysipelas. For more information on boosting the immune system and maintaining overall health, refer to our article on strengthening the immune system.
By recognizing these triggers and taking necessary precautions, individuals with erysipelas can reduce the frequency and severity of outbreaks. It’s essential to work closely with healthcare professionals to develop a comprehensive management plan that addresses these triggers and promotes overall skin health.
Preventive Measures for Erysipelas
While treating erysipelas is essential, taking preventive measures can help reduce the risk of developing this skin infection. By incorporating the following practices into your routine, you can minimize the likelihood of erysipelas occurrence.
Maintaining Good Skin Hygiene
Maintaining good skin hygiene is crucial in preventing erysipelas. Regularly washing your skin with mild soap and warm water helps remove dirt, bacteria, and other impurities that can contribute to skin infections. Pay extra attention to areas prone to moisture accumulation, such as skin folds, and ensure they are kept clean and dry.
Additionally, moisturizing your skin with a gentle, non-irritating lotion or cream helps maintain skin health and reduces the risk of dryness and cracks, which can provide an entry point for bacteria. Choose products that are suitable for your skin type and avoid using harsh chemicals that can disrupt the skin’s natural balance.
Treating Skin Injuries Promptly
Promptly treating any skin injuries, such as cuts, scrapes, or insect bites, can help prevent the development of erysipelas. Clean the affected area with antiseptic solutions and cover it with a sterile bandage or dressing to protect it from bacteria and other contaminants.
Avoid delaying treatment for skin injuries, as even minor wounds can provide an opportunity for bacteria to invade the skin and cause infection. If you notice any signs of redness, swelling, or warmth around a skin injury, seek medical attention promptly to prevent the infection from spreading.
Strengthening the Immune System
A strong immune system plays a vital role in preventing various infections, including erysipelas. To strengthen your immune system, practice a healthy lifestyle that includes:
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. These provide essential nutrients and antioxidants that support immune function.
- Staying physically active to improve overall health and immune system function.
- Getting enough sleep to allow your body to repair and regenerate cells, including immune cells.
- Minimizing stress through relaxation techniques, exercise, and engaging in activities you enjoy.
- Avoiding smoking and excessive alcohol consumption, as these can weaken the immune system.
By maintaining good skin hygiene, promptly treating skin injuries, and strengthening your immune system, you can reduce the risk of erysipelas and promote overall skin health. Remember, if you suspect any signs or symptoms of erysipelas, consult a healthcare professional for proper diagnosis and treatment.
Seeking Medical Attention
If you suspect that you have erysipelas or are experiencing symptoms associated with this condition, it is important to seek medical attention. A healthcare professional can provide an accurate diagnosis and recommend appropriate treatment options.
When to Consult a Healthcare Professional
It is advisable to consult a healthcare professional if you experience any of the following:
-
Persistent Symptoms: If your symptoms persist or worsen despite self-care measures, it is essential to seek medical attention. This may include symptoms such as persistent redness, swelling, pain, or fever.
-
Spreading Infection: If the infection appears to be spreading rapidly or affecting a larger area of the skin, it is crucial to consult a healthcare professional promptly. They can assess the severity of the infection and provide appropriate treatment.
-
Underlying Health Conditions: Individuals with certain underlying health conditions, such as diabetes or compromised immune systems, may be at higher risk for complications from erysipelas. It is important for them to consult a healthcare professional for proper evaluation and management.
Diagnostic Tests for Erysipelas
In order to confirm a diagnosis of erysipelas, a healthcare professional may perform several diagnostic tests, which may include:
-
Physical Examination: A healthcare professional will typically start by conducting a thorough physical examination of the affected area. They will assess the appearance of the skin, check for characteristic symptoms such as redness and swelling, and evaluate any associated symptoms.
-
Blood Tests: Blood tests may be ordered to check for signs of infection, such as elevated white blood cell count or increased levels of inflammatory markers. These tests can help confirm the diagnosis and assess the severity of the infection.
-
Cultures: In some cases, a healthcare professional may take a sample of the affected skin, such as a swab or a biopsy, for laboratory testing. This can help identify the specific bacteria causing the infection and guide appropriate antibiotic treatment.
-
Imaging Studies: In rare instances, imaging studies such as ultrasound or magnetic resonance imaging (MRI) may be recommended to evaluate the extent of the infection or to rule out any underlying abscess formation.
By consulting a healthcare professional and undergoing the necessary diagnostic tests, you can receive an accurate diagnosis of erysipelas and begin appropriate treatment. Remember, early intervention is key in managing this condition effectively and reducing the risk of complications.
Coping with Erysipelas and Finding Relief
When faced with the discomfort and inflammation caused by erysipelas, it’s important to explore treatment options and adopt self-care measures to find relief. By addressing the underlying causes and managing the symptoms, individuals can effectively cope with erysipelas.
Treatment Options for Erysipelas
The primary treatment approach for erysipelas involves the use of antibiotics to combat the bacterial infection. These antibiotics may be prescribed in oral or intravenous form, depending on the severity of the infection. It’s crucial to complete the full course of antibiotics as prescribed by a healthcare professional to ensure the infection is fully eradicated.
In addition to antibiotics, healthcare providers may recommend pain relievers to alleviate the discomfort associated with erysipelas. Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and swelling.
For more severe cases or situations where complications arise, hospitalization may be necessary. In the hospital setting, intravenous antibiotics and supportive care can be provided to manage the infection effectively.
Self-Care Measures for Symptom Management
Alongside medical treatment, there are several self-care measures that individuals can adopt to manage the symptoms of erysipelas and promote healing:
-
Elevate the affected area: Elevating the affected limb can help reduce swelling and promote better circulation, aiding in the healing process.
-
Apply cool compresses: Cool compresses can help soothe the skin and alleviate discomfort. Simply dampen a clean cloth with cool water and apply it gently to the affected area.
-
Practice good skin hygiene: Keeping the affected area clean and dry is essential for preventing the spread of infection. Follow proper hygiene practices, such as regular handwashing and using gentle cleansers.
-
Avoid tight clothing: Wearing loose-fitting clothing can help prevent irritation and allow for better airflow, aiding in the healing process.
-
Take steps to boost the immune system: A strong immune system plays a crucial role in fighting off infections. Get adequate rest, eat a balanced diet, stay hydrated, and consider incorporating immune-boosting foods and supplements into your routine. For more information on strengthening the immune system, check out our article on boosting the immune system.
It’s important to note that self-care measures should complement medical treatment and not replace it. Always consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan. If symptoms worsen or persist despite treatment, it’s essential to seek prompt medical attention.
By combining medical treatment with self-care measures, individuals can effectively cope with erysipelas and find relief from the symptoms. Remember to follow the guidance of healthcare professionals, practice good skin hygiene, and take steps to support overall health and well-being.
