Published 31 August 2023
Putting an End to the Mystery: Identifying Psoriasis Triggers Made Simple
Understanding Psoriasis Triggers
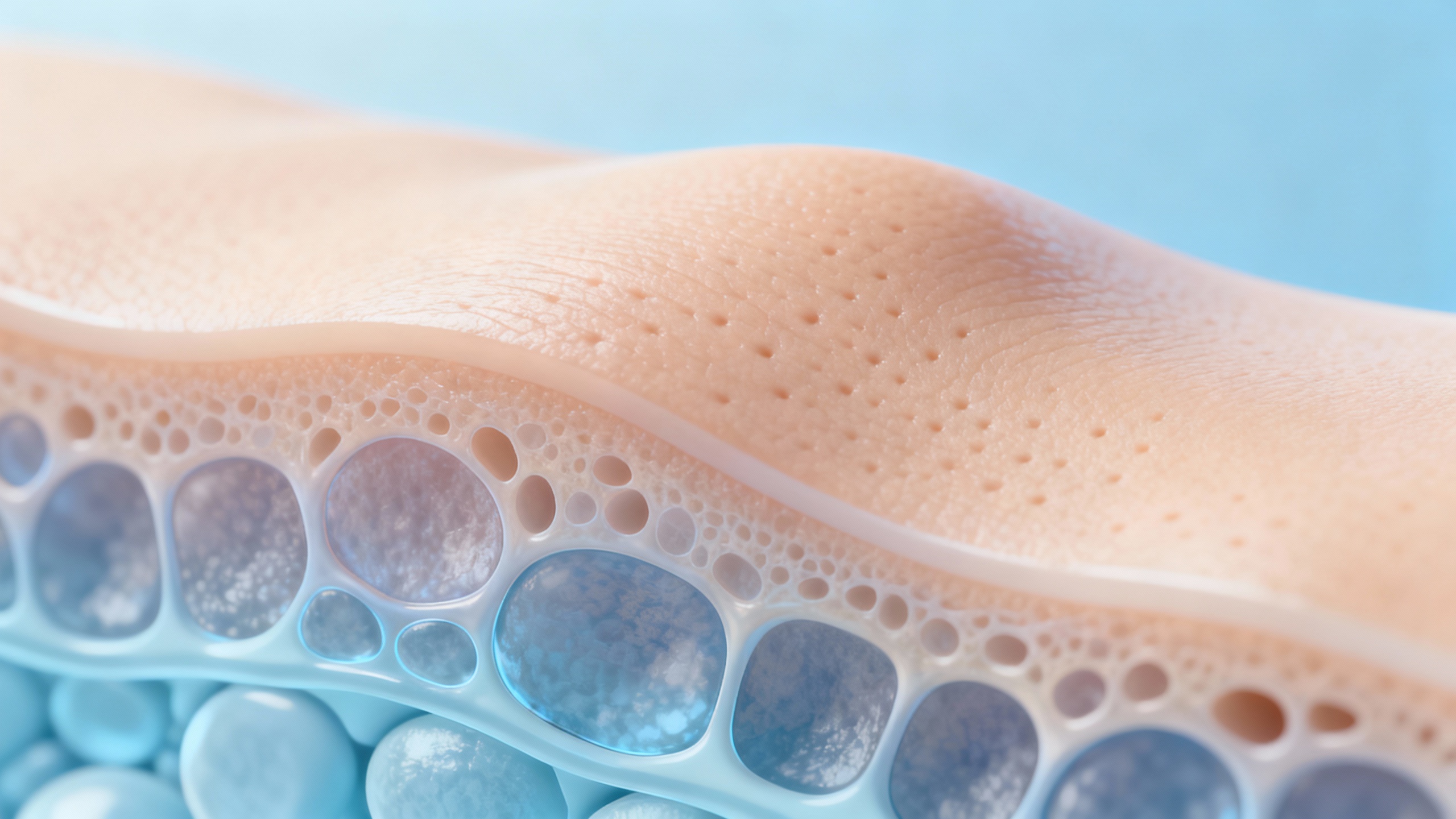
Psoriasis is a chronic skin condition characterized by raised, red, and scaly patches on the skin. Understanding the causes and triggers of psoriasis is essential for managing and minimizing flare-ups. Let’s explore what psoriasis is and the role triggers play in its development.
What is Psoriasis?
Psoriasis is an autoimmune condition that affects the skin cells’ life cycle. In a healthy individual, skin cells go through a cycle of growth and shedding over the course of a month. However, in people with psoriasis, this process is accelerated, causing a buildup of skin cells on the surface. The resulting patches can be itchy, painful, and aesthetically distressing.
Psoriasis can occur on various parts of the body, including the scalp, elbows, knees, and lower back. The severity and extent of the condition can vary significantly from person to person. It can also be influenced by various factors, including genetics, immune system dysfunction, and environmental triggers.
The Role of Triggers in Psoriasis
Psoriasis is a complex condition influenced by multiple triggers. Triggers are external or internal factors that can activate or worsen psoriasis symptoms. While triggers can vary from person to person, some common ones include:
-
Stress and Emotional Factors: Emotional stress, anxiety, and trauma can trigger or exacerbate psoriasis symptoms. Managing stress through relaxation techniques and seeking emotional support can help reduce flare-ups.
-
Weather and Climate: Changes in weather conditions, particularly cold and dry environments, can trigger psoriasis symptoms. Dry air can cause skin dryness and irritation, leading to flare-ups. Protective measures, such as using moisturizers and wearing appropriate clothing, can help manage symptoms during different seasons.
-
Infections and Illnesses: Infections, such as strep throat or respiratory infections, can trigger or worsen psoriasis symptoms. It’s important to promptly treat any infections and take preventive measures to minimize their impact on psoriasis.
-
Medications and Treatments: Certain medications, such as beta-blockers and lithium, can trigger or worsen psoriasis symptoms in some individuals. Discussing medication options with a healthcare professional and informing them about your psoriasis condition can help find suitable alternatives when necessary.
-
Lifestyle Factors: Unhealthy lifestyle habits, including smoking, excessive alcohol consumption, and poor diet, can contribute to the development and worsening of psoriasis. Making healthy choices, such as maintaining a balanced diet and engaging in regular physical activity, can help manage psoriasis symptoms.
By identifying and understanding these triggers, individuals with psoriasis can take proactive steps to manage their condition more effectively. It is important to note that triggers can vary from person to person, and what may trigger one person’s psoriasis may not affect another’s. Keeping a symptom journal and consulting with a healthcare professional can help identify personal triggers and develop tailored strategies for managing psoriasis effectively.
Common Psoriasis Triggers
Psoriasis, a chronic autoimmune skin condition, can be influenced by various triggers. By understanding and identifying these triggers, individuals with psoriasis can better manage their symptoms and reduce flare-ups. Some common psoriasis triggers include stress and emotional factors, weather and climate, infections and illnesses, medications and treatments, and lifestyle factors.
Stress and Emotional Factors
Stress and emotional factors play a significant role in triggering psoriasis flare-ups. High levels of stress can lead to the release of certain chemicals in the body that may exacerbate inflammation and worsen psoriatic symptoms. Emotional factors such as anxiety, depression, and trauma can also impact the immune system and contribute to psoriasis flare-ups. By implementing stress management techniques like meditation, yoga, and therapy, individuals with psoriasis can potentially reduce the frequency and severity of flare-ups.
Weather and Climate
Weather and climate changes can have a profound impact on psoriasis symptoms. Cold and dry weather conditions can cause the skin to become dry and flaky, leading to increased inflammation and itchiness. On the other hand, hot and humid climates can trigger excessive sweating and irritation in individuals with psoriasis. Protective measures such as using moisturizers, wearing appropriate clothing, and avoiding extreme temperatures can help manage psoriasis symptoms related to weather changes.
Infections and Illnesses
Infections and illnesses can act as triggers for psoriasis flare-ups. Common infections like strep throat, respiratory infections, and skin infections can cause the immune system to become overactive, triggering psoriasis symptoms. Additionally, certain chronic illnesses like autoimmune disorders and HIV/AIDS are known to be associated with psoriasis. By taking steps to prevent infections and seeking prompt treatment for any underlying illnesses, individuals with psoriasis can potentially reduce the risk of flare-ups.
Medications and Treatments
Certain medications and treatments can worsen or trigger psoriasis symptoms. Some drugs, including lithium, beta-blockers, and antimalarial drugs, have been linked to psoriasis flare-ups. Additionally, abruptly stopping or withdrawing from systemic corticosteroids can induce a rebound effect, leading to a sudden onset or worsening of psoriasis symptoms. It is important for individuals with psoriasis to communicate with their healthcare providers about their condition and discuss any potential side effects or interactions that may impact their psoriasis.
Lifestyle Factors
Lifestyle factors, such as smoking, excessive alcohol consumption, and poor diet, can contribute to psoriasis flare-ups. Smoking has been shown to increase the risk of developing psoriasis and worsen existing symptoms. Excessive alcohol consumption can also trigger or exacerbate psoriasis. A well-balanced diet, rich in nutrient-dense foods, can help support overall skin health and potentially reduce psoriasis symptoms. Making healthy lifestyle choices, including maintaining a healthy weight, getting regular exercise, and avoiding triggers like smoking and excessive alcohol, can play a significant role in managing psoriasis.
By identifying and understanding these common psoriasis triggers, individuals can take proactive steps to manage their condition. It is essential to work closely with healthcare professionals to develop an individualized treatment plan that addresses both the underlying causes and the symptoms of psoriasis. With the right strategies in place, individuals with psoriasis can seek relief and live a healthier, more comfortable life.
Identifying Your Personal Psoriasis Triggers
Psoriasis triggers can vary from person to person, making it important to identify your specific triggers in order to effectively manage your condition. By understanding what factors contribute to your psoriasis flare-ups, you can take proactive steps to minimize their impact on your skin. Here are three strategies to help you identify your personal psoriasis triggers:
Keeping a Symptom Journal
Keeping a symptom journal can be a valuable tool in identifying your psoriasis triggers. Record any changes in your skin, such as flare-ups, itching, or redness, along with potential triggers or events that may have preceded them. This can include information about your diet, stress levels, weather conditions, medication changes, or any other factors that you suspect may be influencing your psoriasis. Over time, patterns may emerge, helping you pinpoint specific triggers. This information can also be helpful when discussing your condition with a healthcare professional.
Consulting with a Healthcare Professional
Working closely with a healthcare professional is essential in identifying and managing your psoriasis triggers. Dermatologists, in particular, specialize in diagnosing and treating skin conditions like psoriasis. They can help you identify potential triggers and provide guidance on how to manage them effectively. A dermatologist may also recommend additional tests or examinations to assess other possible underlying causes of your psoriasis symptoms.
Conducting Patch Testing
In some cases, conducting patch testing may be beneficial to identify triggers that could be causing or exacerbating your psoriasis. Patch testing involves applying small amounts of various substances to your skin, typically on your back, and monitoring for any allergic reactions or skin irritations. This can help identify specific allergens or irritants that may be contributing to your psoriasis flare-ups. However, it’s important to note that not all psoriasis cases are triggered by allergies or irritants.
By implementing these strategies, you can gain valuable insights into the factors that trigger your psoriasis. Remember to be patient and persistent, as identifying triggers may take time and involve trial and error. Once you have a better understanding of your personal triggers, you can take proactive steps to manage and minimize their impact on your skin.
To learn more about managing psoriasis triggers and other skin conditions, visit our articles on food allergies and skin rashes, skin rash causes and treatment, and autoimmune disorders and skin rashes.
Strategies for Managing Psoriasis Triggers
Managing psoriasis triggers is essential for minimizing flare-ups and maintaining healthier skin. By implementing effective strategies, individuals with psoriasis can better control their symptoms and improve their quality of life. Here are some key strategies to consider:
Stress Management Techniques
Stress is known to be a common trigger for psoriasis flare-ups. Implementing stress management techniques can help reduce the impact of stress on the skin. Some effective techniques include:
- Meditation: Engaging in mindfulness meditation can help calm the mind and reduce stress levels.
- Exercise: Regular physical activity, such as yoga or aerobics, can help alleviate stress and promote overall well-being.
- Therapy: Seeking therapy or counseling can provide support and help individuals develop effective coping mechanisms for managing stress.
Protective Measures for Weather Changes
Weather and climate changes can have a significant impact on psoriasis symptoms. Taking protective measures during extreme weather conditions can help minimize flare-ups. Consider the following:
- Moisturize: Regularly moisturize the skin to prevent dryness and maintain its natural barrier.
- Sun Protection: Apply a broad-spectrum sunscreen with a high SPF to protect the skin from harmful UV rays.
- Hydration: Drink plenty of water to keep the skin hydrated, especially during hot and dry weather.
Preventing Infections and Illnesses
Infections and illnesses can trigger psoriasis flare-ups. Taking preventive measures to avoid infections and maintain overall health is crucial. Consider the following steps:
- Hand Hygiene: Practice regular handwashing to reduce the risk of infections.
- Avoid Sick Individuals: Minimize contact with individuals who have contagious illnesses to reduce the likelihood of getting sick.
- Maintain a Healthy Lifestyle: Follow a balanced diet, get enough sleep, and engage in regular exercise to support a strong immune system.
Working with Healthcare Providers
Collaborating with healthcare providers is essential for managing psoriasis triggers effectively. They can provide personalized guidance and treatment options tailored to individual needs. Some key considerations include:
- Regular Check-ups: Schedule regular check-ups with a dermatologist to monitor your condition and discuss any concerns.
- Medication Review: Discuss any medications you are taking with your healthcare provider, as certain medications can trigger or worsen psoriasis symptoms.
- Treatment Plan: Work with your healthcare provider to develop a comprehensive treatment plan that addresses both the underlying condition and trigger management.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle is fundamental for managing psoriasis triggers. Making positive choices can positively impact the overall well-being and reduce the likelihood of flare-ups. Consider the following:
- Nutritious Diet: Follow a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to provide essential nutrients for skin health.
- Avoid Smoking: Smoking can exacerbate psoriasis symptoms and hinder the effectiveness of treatment. Quitting smoking can have numerous health benefits.
- Limit Alcohol Consumption: Excessive alcohol consumption can trigger or worsen psoriasis symptoms. Limiting alcohol intake can help manage flare-ups.
By implementing these strategies, individuals with psoriasis can take proactive steps to identify and manage their triggers effectively. However, it’s important to consult with a healthcare professional for personalized advice and guidance. For more information on skin rashes and triggers, you can refer to our article on identifying contact dermatitis triggers.
Seeking Relief for Psoriasis Symptoms
Psoriasis, a chronic skin condition characterized by red, scaly patches on the skin, can be managed and its symptoms alleviated through various treatment options. Some of the common methods for seeking relief from psoriasis symptoms include topical treatments, phototherapy, systemic medications, and alternative and complementary therapies.
Topical Treatments
Topical treatments are often the first line of defense for managing mild to moderate psoriasis symptoms. These treatments are applied directly to the affected areas of the skin and can help reduce inflammation, control itching, and promote the healing of psoriatic plaques.
Common topical treatments for psoriasis include corticosteroids, vitamin D analogues, retinoids, and salicylic acid. These medications work by suppressing the immune response and slowing down the excessive growth of skin cells. It’s important to note that the choice of topical treatment depends on the severity and location of the psoriasis plaques. Consulting with a healthcare professional is essential to determine the most suitable treatment for your specific condition.
Phototherapy
Phototherapy, also known as light therapy, involves exposing the skin to ultraviolet (UV) light in a controlled manner. This treatment is particularly effective for individuals with moderate to severe psoriasis or those who have not responded well to topical treatments.
During phototherapy, the affected skin is exposed to either natural sunlight or artificial UV light. This exposure helps to slow down the rapid growth of skin cells and reduce inflammation. Phototherapy can be performed under medical supervision in specialized clinics or with the use of home phototherapy units.
Systemic Medications
In cases of severe psoriasis or when topical treatments and phototherapy are not sufficient, systemic medications may be prescribed. These medications work internally to target the underlying cause of psoriasis and reduce inflammation throughout the body.
Systemic medications for psoriasis include oral medications, such as methotrexate, cyclosporine, and acitretin, as well as biologic drugs that are injected or administered intravenously. Biologics specifically target molecules involved in the immune system response, thereby reducing inflammation and controlling psoriasis symptoms.
It is important to note that systemic medications for psoriasis may have potential side effects and require close monitoring by a healthcare professional. Regular follow-ups and discussions with your healthcare provider are crucial to ensure the benefits outweigh any potential risks.
Alternative and Complementary Therapies
In addition to conventional treatments, some individuals with psoriasis explore alternative and complementary therapies to help manage their symptoms. These therapies may include herbal remedies, acupuncture, dietary changes, and mind-body techniques such as meditation and yoga.
While there is limited scientific evidence supporting the effectiveness of these therapies for psoriasis, some individuals may find them beneficial as adjuncts to their primary treatment. It is essential to consult with a healthcare professional before incorporating alternative and complementary therapies into your psoriasis management plan to ensure they are safe and compatible with your current treatment regimen.
By exploring different treatment options, individuals with psoriasis can find relief from their symptoms and improve their overall quality of life. It’s important to work closely with a healthcare professional to develop a personalized treatment plan tailored to your specific needs. Remember, what works for one person may not work for another, so finding the right combination of treatments may require some trial and error.
